Researchers Investigate Drug Resistant Ovarian Cancer to Improve Clinical Treatment
Posted on: 03 August 2012
A new study by TCD researchers investigates drug-resistant ovarian cancer cells. The findings which have been recently published in the international publication, PLoS One will increase understanding of molecular markers in drug-resistant ovarian cancer with a view to improving clinical treatment.
Worldwide there are more than 204,000 new cases of ovarian cancer each year, accounting for around 4% of all cancers diagnosed in women. For many cancers, including ovarian, chemotherapy remains the only treatment option. While chemotherapy has its success stories, the majority of ovarian cancer patients will go on to develop chemotherapy-resistant disease. Determining which chemotherapy drug to give a patient is a complicated process. Most decisions are made based on the type of cancer the patient has and how advanced it is. Currently, there is a shift towards individually tailoring chemotherapy to each patient. A personalised approach has improved treatment outcomes in breast cancer by targeting therapy according to its subtype.
In the case of ovarian cancer, research fellow and lead author Dr Britta Stordal says: “If we can subdivide ovarian cancer patients into different resistance categories we can start personalising the treatment of this disease. The cost of patients receiving chemotherapy that they do not respond to is high, both personally for the patients and financially for the healthcare system. By understanding how chemotherapy resistance develops in ovarian cancer we can determine the best drug to prescribe to each patient. The individual tailoring of chemotherapy for relapsed patients can only improve cancer treatment in terms of increased response rates. “
The research studies drug-resistant ovarian cancer cells called IGROVCDDP. The cells were originally developed in a laboratory in the Netherlands. IGROV-1 cells, were firstly derived from an ovarian cancer patient. IGROV-1 cells were put through cycles of chemotherapy in the laboratory to simulate what a cancer patient receives in the clinic. The daughter cells produced are the IGROVCDDP cells, which were grown in tissue culture and examined as to how they became drug resistant.
IGROVCDDP cells are resistant to the two chemotherapy drugs used in the first line treatment of ovarian cancer, cisplatin and paclitaxel. By studying the IGROVCDDP cells we can identify genes and proteins that have changed and may be useful as molecular markers of chemotherapy resistance in the clinic. IGROVCDDP cells have many molecular markers of chemotherapy resistance and highlight the multiple mechanisms that can exist simultaneously in drug-resistant cancer cells. IGROVCDDP cells have increased levels of the drug-efflux pump, P-glycoprotein. This causes resistance to paclitaxel by pumping the drug out of the cancer cell. The study highlights that the P-glycoprotein can co-exist with multiple mechanisms of resistance to cisplatin. Cisplatin resistance is mediated in part by detoxification by the glutathione pathway and decreased uptake of drug into the cell. This is a step towards understanding how molecular markers of drug resistance interact and overlap in in ovarian cancer patients.
“We will now go on to examine molecular markers identified in IGROVCDDP in samples of tumours from ovarian cancer patients. Hopefully we will find markers that can separate patients who respond and those who do not respond to cisplatin and paclitaxel chemotherapy. Patients we think that will respond could be given the standard cisplatin/paclitaxel chemotherapy, and those who have a poor chance of responding could be given alternative treatment,” concluded Dr Stordal.
Full title of paper: Paper published in PLoS One – “Resistance to Paclitaxel in a Cisplatin-Resistant Ovarian Cancer Cell Line Is Mediated by P-Glycoprotein”
Funding was received from the Irish Cancer Society and a Marie Curie Reintegration Grant FP7. The work was also funded by a Marie Curie International Incoming Fellowship FP7 and supported by a travel fellowship from the European Association of Cancer Research. The work was conducted in a laboratory funded by The Emer Casey Foundation as part of the DISCOVARY consortium.
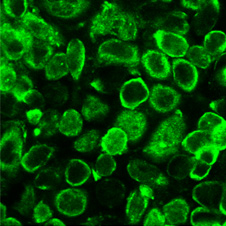
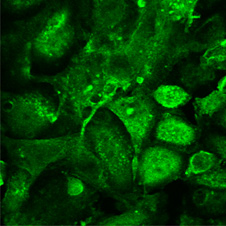
Microscope images of CTR1, which is a cisplatin uptake transporter in drug resistant ovarian cancer cells IGROV-1 (left) and CDDP
