The impact of COVID-19 on maternity care
Ms Paula Barry, Ms Nora Vallejo: Coombe Women and Infants University Hospital
Funding: Trinity College Dublin’s Office of the Dean of Research COVID-19 Response Fund
Background
In March of 2020, the first of a series of national lockdowns was implemented in Ireland as a means of reducing the community spread of COVID-19. This resulted in changes to maternity care practices that had the potential to impact on the clinical and experiential outcomes of women accessing maternity care during this time. Some of these changes included policies of restrictive visiting (e.g. one designated parent for babies in the neonatal intensive care unit, no visiting on antenatal, postnatal and gynaecology wards), reconfiguration of physical space to accommodate suspected or confirmed cases of women who were COVID-19 positive, suspension of key services such as parent education, antenatal classes and birth reflection clinics, increased antenatal and postnatal telephone consultations, and displacement of some outreach antenatal clinics back to the hospital.
To explore the impact of COVID-19 on maternity care, we evaluated both clinical and experiential outcomes in a two-phase study at one hospital site in Ireland. Phase 1 involved a comparative review of maternal clinical outcomes four months before and four months during implementation of COVID-19 maternity care practice changes at the hospital. Phase 2 involved interviews with 19 women to gain an understanding of their experiences of maternity care during COVID-19. In this report we provide some of the key findings from phase 1. Phase 2 findings are currently being analysed and will be reported separately.
Methods
The study design was a before and during comparative audit of clinical outcome data in women attending an urban, tertiary referral maternity hospital that has an annual birth rate of >8000 births per year. Ethical approval for the study was granted by the University and Hospital Research Ethics Committees. Information on women’s clinical outcomes (e.g. labour induction, mode of birth, initiation of breast feeding, length of postnatal stay, admission to NICU and readmission rates), recorded as part of routine hospital care, were collected from the hospital electronic information system. Data were collected in August 2020, and the periods of relevance to the study were from mid-Dec 2019 to mid-March 2020 (before COVID-19 cohort) and from mid-March to mid-July 2020 (during COVID-19 cohort). Data were comparatively analysed and reported as frequencies and proportions. Z-tests were used to compare proportions with alpha set at 0.05.
Results
Data on 4886 women who gave birth at the study site were analysed (Table 1).
Table 1: Summary details of numbers included in the study
Before Group |
During Group |
|||||||||
Total no. of women who gave birth |
Total no of women who gave birth |
|||||||||
16-Nov 2019 to 15-March 2020 |
16-March 2020 to 15-July 2020 |
|||||||||
M1 |
M2 |
M3 |
M4 |
Total |
M1 |
M2 |
M3 |
M4 |
Total |
|
Primiparous |
277 |
270 |
288 |
249 |
1084 |
248 |
236 |
235 |
247 |
966 |
Multiparous |
333 |
363 |
346 |
315 |
1357 |
321 |
375 |
389 |
394 |
1479 |
Totals |
610 |
633 |
634 |
564 |
2441 |
569 |
611 |
624 |
641 |
2445 |
M=Month; Primiparous - first time mothers; Multiparous - women who have given birth previously
Caesarean birth
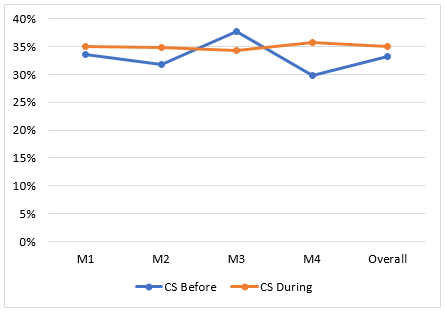
Overall, the rate of caesarean section (CS) remained stable throughout the before and during COVID-19 periods (33% vs 35%, p=0.4). The CS rates each month during COVID, however, appeared more stable compared to the pre-COVID months (Figure 1).
Figure 1 (above): Caesarean birth overall
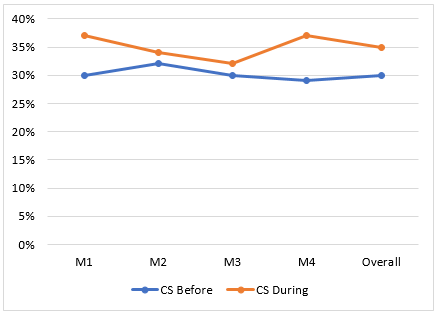
When CS rates were analysed separately by parity, however, an increased CS rate was observed in multiparous women during COVID-19 compared to before COVID-19 (30% vs 35%, p=0.01, Figure 2). CS in primiparous women was decreased from 37% to 35%, but this difference was not significant (p=0.4).
Figure 2 (above): Caesarean birth in multiparous women
Comparing emergency and elective (planned) CS as part of overall CS rates from before and during COVID periods revealed an increased elective CS rate during COVID-19. This split had been relatively balanced before COVID-19 (Table 2).
Table 2: Elective versus Emergency CS as proportions of overall CS
|
Elective CS |
Emergency CS |
Z score (p-value) |
Before COVID |
48.2% |
51.8% |
-1.1 (0.27) |
During COVID |
43.2% |
56.8% |
-4.4 (<0.0001) |
Concomitant changes in spontaneous vaginal birth (SVB) and assisted vaginal birth (AVB) (i.e. assisted means with the help from a doctor using a forceps or vacuum instrument) were also observed between the two time periods, but these changes were not significantly different; SVB 56% vs 52%, p=0.15 and AVB 12% vs 13%, p=0.3.
Other intrapartum outcomes: Although induction of labour (IOL) overall remained stable across the two time periods, post-maturity IOL, defined as IOL at ≥Term +10 days, significantly increased during COVID-19 (Table 3). Statistically significant increases were also observed in augmentation of labour (i.e. speeding up labour by breaking a woman’s waters or giving a drug called syntocinon to increase the rate and strength of labour contractions) following spontaneous onset of labour (SOL) in the immediate-term following COVID-19 (month 1), but not overall (Table 3).
Table 3: Other intrapartum outcomes
Variable |
% - Before |
% – During |
P-values |
IOL overall |
37.6% |
36.9% |
0.65 |
IOL post-maturity |
12.4% |
16.7% |
0.007* |
Augmentation of labour following SOL |
18.4% |
20.1% |
0.4 |
Epidural analgesia |
41.6% |
40.1% |
0.3 |
*significant p<0.05
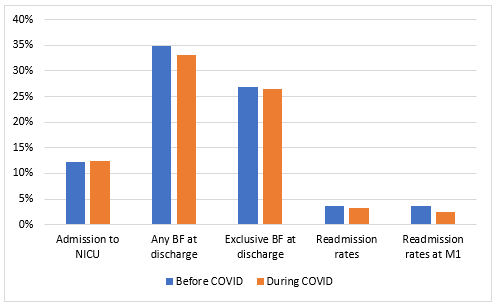
Postnatal outcomes: Figure 3 presents the results for some key postnatal outcomes. No differences were observed in the outcomes of admission to neonatal intensive care, breastfeeding at discharge and postpartum readmission rates.
Figure 3 (above): Postnatal outcomes
Conclusion
Practice changes implemented as a result of COVID 19, in general, have affected relatively few maternal clinical outcomes, although those affected have the potential to impact considerably on women’s intrapartum and postpartum health and wellbeing. Such outcomes included proportionally increased elective compared to emergency CS rates, increased CS in multiparous women, increased augmentation of labour and increased rates of IOL for post-dates. Further exploration is warranted to explain these findings, but practices related to controlling the environment following lockdown may have been influential drivers. For example, the increased elective compared to emergency CS rate and the increase in CS in multiparous women may be interlinked. Due to the pandemic, women with previous CS may have been more inclined, or may have been advised to opt for an elective repeat CS rather than planned vaginal birth after CS. This might be because the former allows for scheduling and thus a degree of control over maternity admissions during the lockdown period. Irrespective of possible reasons, having awareness of these findings can be helpful as the COVID-19 pandemic continues. This will help ensure that any practice changes implemented as a result of COVID-19 are not inadvertently impacting negatively on women’s labour, birth and postpartum outcomes.
Acknowledgements
We are grateful for funding from Trinity College Dublin’s Office of the Dean of Research COVID-19 Response Fund which supported this valuable study. We sincerely thank E. McNamee in the IT Department of the study site who assisted in providing us with the collated, anonymous clinical outcome data.
Valerie Smith
Valerie Smith is a Professor in Midwifery at the School of Nursing and Midwifery, and a registered General Nurse, Midwife and Clinical Nurse Teacher. Valerie's research interests extend to all areas of maternity care and healthcare research methods, with specific topic expertise in the areas of antenatal and intrapartum fetal wellbeing, intrapartum care (mode of birth, perineal care) and postnatal morbidity. Valerie's areas of methodological research expertise include systematic reviews, randomised trial research, survey research, and qualitative research methods. Valerie is a Cochrane Ireland and UK Senior systematic review trainer, a member of three HRB-Clinical Trial Networks, an Executive Committee member of Evidence Synthesis Ireland (ESI), and a member of the international collaborative Trials Methodology Research Partnership (Outcomes Working Group). In addition to PhD supervision, Valerie has previously mentored two HRB Cochrane Fellows and one ESI Fellow to project completion and is currently mentoring two ESI Fellows. As a practitioner, teacher and researcher, Valerie is passionate about advancing healthcare knowledge, practice and research, and in capacity building for excellence in these areas.
- Follow Valerie on Twitter
- Find Valerie on ResearchGate
- Read Part 2 of this study
- Maternity Care during Covid-19
- School of Nursing & Midwifery
- Research Groups
- THE Conference 2021